 IJCP Editorial Team
IJCP Editorial Team
Meningococcemia Presenting with Purpura Fulminans and Pericardial Involvement
Abstract
Purpura fulminans (PF) is a rapidly progressive thrombotic disorder of the dermal microvasculature associated with disseminated intravascular coagulation (DIC) and high mortality. Meningococcemia is a well-recognized cause of PF, but cardiac complications are rare. We report a case of meningococcal pericarditis in the setting of PF, highlighting diagnostic and therapeutic challenges.
Keywords: Purpura fulminans, meningococcemia, pericarditis, pericardial effusion, Neisseria meningitidis.
Introduction
Purpura fulminans is a dermatologic emergency characterized by the sudden appearance of petechiae, ecchymoses, and skin necrosis due to acute small-vessel thrombosis. It most commonly occurs in association with severe bacterial sepsis, particularly Neisseria meningitidis. Cardiac involvement in meningococcal disease is uncommon, with pericarditis reported in <1% of cases. We present a rare case of meningococcal pericarditis complicating PF in a young adult.
Case Presentation
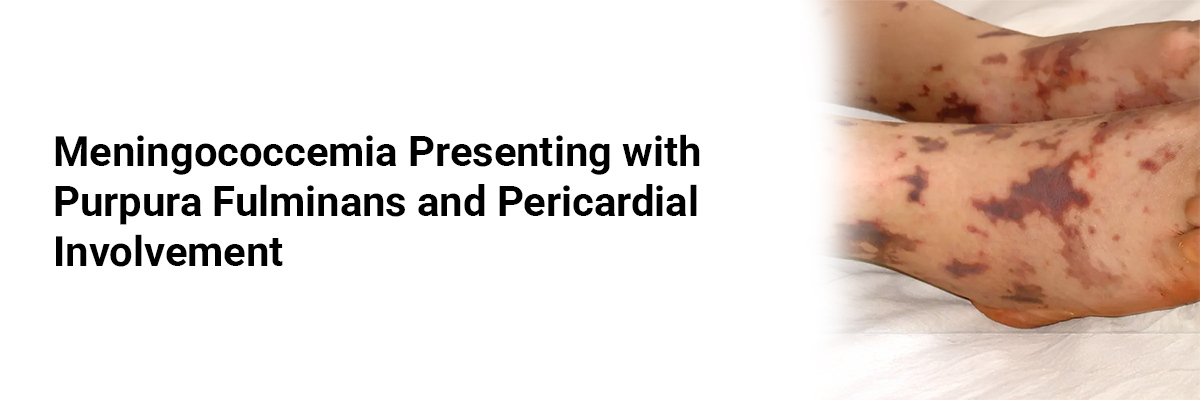
A 19-year-old previously healthy male presented to the emergency department with a 24-hour history of high-grade fever, chills, diffuse myalgia, and a rapidly spreading purpuric rash over the lower limbs and trunk. He also reported chest discomfort and shortness of breath for the last 6 hours.
On examination, the patient was febrile (39.8 °C), hypotensive (BP 84/52 mmHg), tachycardic (HR 128 bpm), and tachypneic (RR 28/min) with oxygen saturation of 92% on room air. Purpuric, non-blanching skin lesions were noted over the extremities, with some areas showing early necrosis. Cardiovascular examination revealed muffled heart sounds; jugular venous distension was present.
Laboratory investigations showed leukocytosis (WBC 18,500/mm³), thrombocytopenia (platelets 64,000/mm³), elevated D-dimer, prolonged PT/INR, and low fibrinogen—findings consistent with DIC. Blood cultures grew Neisseria meningitidis (serogroup C) within 24 hours.
Echocardiography demonstrated a moderate pericardial effusion with echocardiographic signs of early tamponade. Chest X-ray showed an enlarged cardiac silhouette.
Management and Outcome
The patient was admitted to the intensive care unit and managed with intravenous ceftriaxone (2 g every 12 hours), aggressive fluid resuscitation, and inotropic support. Low-dose corticosteroids were initiated for suspected adrenal involvement. Pericardiocentesis was performed, draining 350 mL of serosanguinous fluid; culture of the pericardial fluid was sterile, consistent with immune-mediated pericarditis secondary to meningococcal infection.
For PF, the patient received supportive wound care and prophylactic anticoagulation once coagulopathy improved. Over the following week, his hemodynamics stabilized, the rash began to resolve, and repeat echocardiography showed minimal residual pericardial fluid. He was discharged after 14 days with full recovery and no recurrence on follow-up at 6 weeks.
Discussion
Meningococcal pericarditis may present in three forms: (1) as part of fulminant septicemia, (2) during convalescence as an immune-mediated process, or (3) in the absence of systemic meningococcal disease. In this patient, pericarditis likely represented an early immune-mediated manifestation in the setting of overwhelming meningococcemia and PF.
PF results from a complex interplay of bacterial endotoxins, cytokine storm, and consumption of natural anticoagulants (protein C, protein S, antithrombin III), leading to microvascular thrombosis. Cardiac involvement in PF is rare but clinically significant due to the risk of tamponade and hemodynamic collapse.
Prompt recognition, targeted antibiotic therapy, hemodynamic support, and timely pericardial drainage are crucial for favorable outcomes.
Conclusion
This case underscores the need for heightened clinical suspicion for cardiac complications in patients with meningococcemia and purpura fulminans. Early echocardiographic evaluation and multidisciplinary management can be lifesaving.
Reference
1. Pace D, Pollard AJ. Meningococcal disease: clinical presentation and sequelae. Vaccine. 2012;30 Suppl 2:B3–B9.
2. Karthikeyan G, et al. Meningococcal pericarditis: an underrecognized entity. Heart. 2003;89(5):544–545.

IJCP Editorial Team
Comprising seasoned professionals and experts from the medical field, the IJCP editorial team is dedicated to delivering timely and accurate content and thriving to provide attention-grabbing information for the readers. What sets them apart are their diverse expertise, spanning academia, research, and clinical practice, and their dedication to upholding the highest standards of quality and integrity. With a wealth of experience and a commitment to excellence, the IJCP editorial team strives to provide valuable perspectives, the latest trends, and in-depth analyses across various medical domains, all in a way that keeps you interested and engaged.






















Please login to comment on this article