 IJCP Editorial Team
IJCP Editorial Team
A Rare Case of Exomphalos Linked to Prenatal Alcohol Exposure
Abstract
Exomphalos (omphalocele) is a congenital anterior abdominal wall defect characterized by herniation of abdominal viscera into the base of the umbilical cord, covered by a membrane consisting of peritoneum and amnion. While genetic abnormalities and chromosomal defects are well-established etiological factors, environmental teratogens, including alcohol, are rarely reported in association with this anomaly. We present a case highlighting the potential link between maternal alcohol consumption during early pregnancy and the occurrence of exomphalos in the neonate.
Introduction
Exomphalos occurs in approximately 1 in 4,000–5,000 live births. It is frequently associated with chromosomal anomalies such as trisomy 13, 18, and 21, and syndromic conditions including Beckwith–Wiedemann syndrome. Environmental risk factors, though less common, have also been implicated. Maternal alcohol consumption, especially during the first trimester, is known to cause a spectrum of developmental abnormalities collectively termed Fetal Alcohol Spectrum Disorders (FASD). However, the association of exomphalos with maternal alcohol use is extremely rare. This case report describes a neonate born with exomphalos following documented maternal alcohol exposure in early pregnancy.
Case Presentation
A 27-year-old gravida 2, para 1 woman presented at 38 weeks’ gestation for delivery. The pregnancy was unbooked and unsupervised. She reported occasional alcohol consumption throughout the first trimester, with cessation thereafter. There was no history of smoking, drug abuse, teratogenic medication use, or significant medical illness.
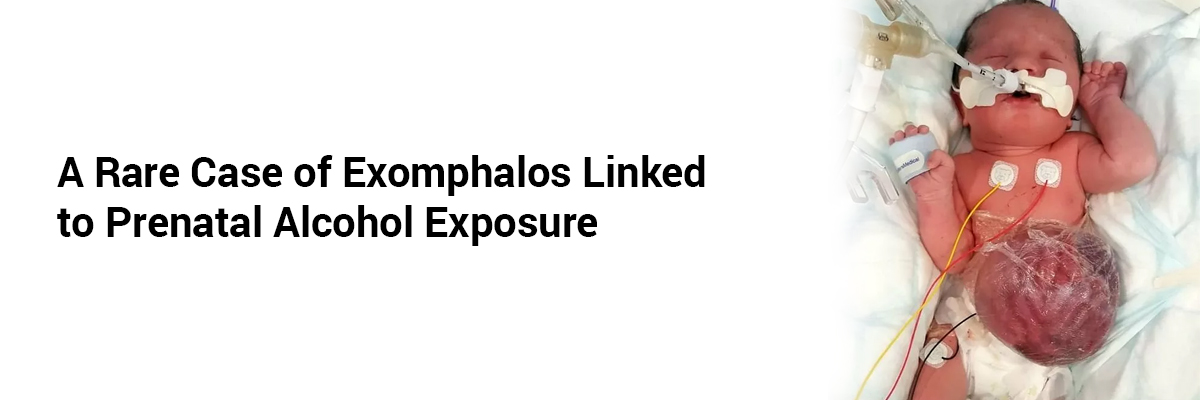
A male neonate weighing 2.6 kg was delivered via spontaneous vaginal delivery. Examination revealed a 5 cm exomphalos sac at the umbilical region containing loops of intestine and part of the liver, covered by a translucent membrane. No other external malformations were noted. The neonate had stable vital signs.
Antenatal ultrasonography performed late in the third trimester had shown a ventral abdominal wall defect but no major internal organ anomalies. Postnatal echocardiography and cranial ultrasonography were normal. Karyotyping revealed a normal 46,XY pattern.
Surgical repair was undertaken on day 2 of life. The postoperative period was uneventful, and the infant was discharged on day 12. The mother was counselled regarding the possible teratogenic effects of alcohol and advised strict abstinence in future pregnancies.
Discussion
Exomphalos results from a failure of the midgut to return to the abdominal cavity during the 10th–12th weeks of gestation. The etiology is multifactorial, involving genetic and environmental influences. Maternal alcohol exposure is a recognized teratogen affecting craniofacial, cardiac, and central nervous system development, but its association with ventral wall defects such as exomphalos remains rarely reported.
Animal studies suggest that ethanol interferes with neural crest cell migration and mesodermal differentiation, potentially disrupting normal morphogenesis of the ventral abdominal wall. The absence of chromosomal abnormalities in this case supports a non-genetic, possibly teratogenic cause.
While causality cannot be definitively established from a single case, this report underscores the need for thorough antenatal counselling regarding alcohol use and heightened vigilance for structural anomalies in pregnancies with known exposure.
Conclusion
This case highlights a rare occurrence of exomphalos in a neonate born to a mother with first-trimester alcohol exposure. Clinicians should consider maternal alcohol consumption as a potential risk factor for abdominal wall defects, and comprehensive prenatal screening and counselling should be emphasized.
References
1. Sadler TW. Langman’s Medical Embryology. 15th ed. Philadelphia: Wolters Kluwer; 2023.
2. Hoyme HE, et al. Updated clinical guidelines for diagnosing fetal alcohol spectrum disorders. Pediatrics. 2016;138(2):e20154256.
3. Bradshaw C, et al. Omphalocele: epidemiology and prenatal diagnosis. Prenat Diagn. 2020;40(10):1253–1262.
4. Sulik KK, et al. Mechanisms of alcohol-induced birth defects: lessons from the mouse. Alcohol Res Health. 2007;30(1):37–47.

IJCP Editorial Team
Comprising seasoned professionals and experts from the medical field, the IJCP editorial team is dedicated to delivering timely and accurate content and thriving to provide attention-grabbing information for the readers. What sets them apart are their diverse expertise, spanning academia, research, and clinical practice, and their dedication to upholding the highest standards of quality and integrity. With a wealth of experience and a commitment to excellence, the IJCP editorial team strives to provide valuable perspectives, the latest trends, and in-depth analyses across various medical domains, all in a way that keeps you interested and engaged.






















Please login to comment on this article