Mycoplasma pneumoniae Pneumonia with Pleural Effusion in a 2-Year-Old Girl
A
report describes a case of a previously healthy 2-year-old girl who presented
with six days of productive cough, high fever, and poor appetite. She was fully
immunized and had no recent travel or sick contacts. On examination, the
patient was febrile (39.2°C), tachypneic (respiratory rate: 42 breaths/min),
mildly hypoxemic (SpO₂ 92–93%), and tachycardic (heart rate: 124 beats/min)
with normal blood pressure (90/60 mmHg). Her weight was 11.9 kg and her height
was 93.5 cm. Lung auscultation was done, and reduced breath sounds in the 1/3
right lower lung were observed, with no additional adventitious sounds. Upon
physical examination, no notable observations were seen.
White
blood cell count (7.9 × 10⁹/L) with 78.7% neutrophils, hemoglobin within normal
limits at 12.1 g/dL, and a reduced platelet count of 137 × 10⁹/L. C-reactive
protein was elevated at 215.6 mg/L while electrolytes, liver function, blood
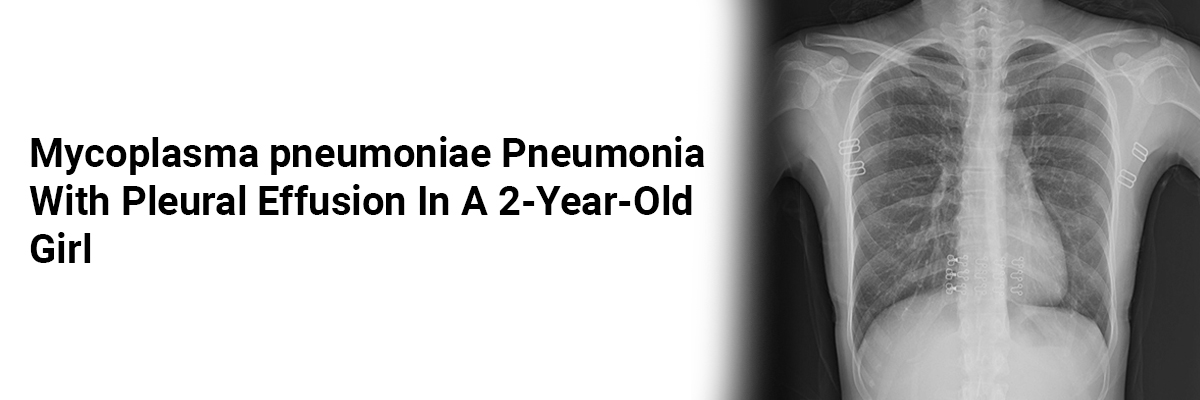
urea nitrogen, and creatinine were all normal. Chest X-ray revealed right lower
lobe consolidation, while thoracic ultrasound showed no pleural effusion. The
patient needed oxygen via nasal cannula for hypoxemic respiratory failure, and
cefotaxime was started empirically for community-acquired pneumonia.
Over
the next three days, she remained febrile (up to 40.1°C) with rising CRP (280
mg/L) and worsening respiratory effort, including subcostal and intercostal
retractions and oxygen saturations of 92–96% on nasal cannula. Blood cultures
were negative. Repeat chest X-ray showed progression of right lower lobe
opacification, and ultrasound detected a small right pleural effusion. Empiric
vancomycin and amikacin were added due to concern for empyema.
Ultrasound-guided
thoracocentesis drained 40 mL of serosanguineous fluid. Analysis confirmed an
exudative fluid with a pleural-to-serum protein ratio of 0.7, a
pleural-to-serum lactate dehydrogenase (LDH) ratio of 1.6, a pleural pH of 7.7,
and a glucose of 82 mg/dL. Cell counts showed 60 WBC/mm³ (90% lymphocytes) and
9,000 RBC/mm³.
PCR
detected 295,000 copies/mL of Mycoplasma
pneumoniae (M. pneumoniae). Blood
cultures did not reveal any growth, and M.
pneumoniae IgM titers rose from 19.9 U/mL on day 3 post-admission to
>150 U/mL within five days. Intravenous levofloxacin was administered for
complicated M. pneumoniae infection;
cefotaxime and amikacin were discontinued, while vancomycin was continued for
seven days. Fever initially subsided but recurred three days later with
increased respiratory distress.
A
chest ultrasound revealed a moderate-to-large right pleural effusion. Later,
170 mL of serosanguineous fluid was drained via pleural effusion, followed by
chest tube placement, which drained an additional 360 mL over 24 hours. Pleural
fluid PCR remained positive for M.
pneumoniae. Following chest tube drainage, her respiratory status improved,
oxygen supplementation was discontinued, and her fever resolved over the next
five days. The chest tube was removed after three days without recurrence of
effusion on ultrasound. The patient completed a 14-day course of levofloxacin
and was discharged after a 16-day hospitalization. At the two-month follow-up,
the patient was doing well, and the chest X-ray showed near-complete resolution
of right lower lobe consolidation.
https://www.ijcripediatrics.com/archive/article-full-text/100012Z19MD2021














Please login to comment on this article