 IJCP Editorial Team
IJCP Editorial Team
A Rare Case Report of Fatal Fulminant Hepatic Failure in a Child
Background
Hepatic dysfunction in malaria has been known for many years, but hepatic encephalopathy is unusual. Jaundice has been found to be more common in falciparum as compared to vivax malaria. According to the WHO, clinical signs of liver failure such as asterixis are almost never seen unless there is concomitant viral hepatitis. Fulminant hepatic failure (FHF), defined as the onset of encephalopathy within 8 weeks of the first symptom of hepatic injury, is commonly due to viral hepatitis or drug use. Severe malaria, defined as jaundice or renal failure with or without altered consciousness, is more common in adults than children and clinically may resemble acute liver failure.
Case Presentation
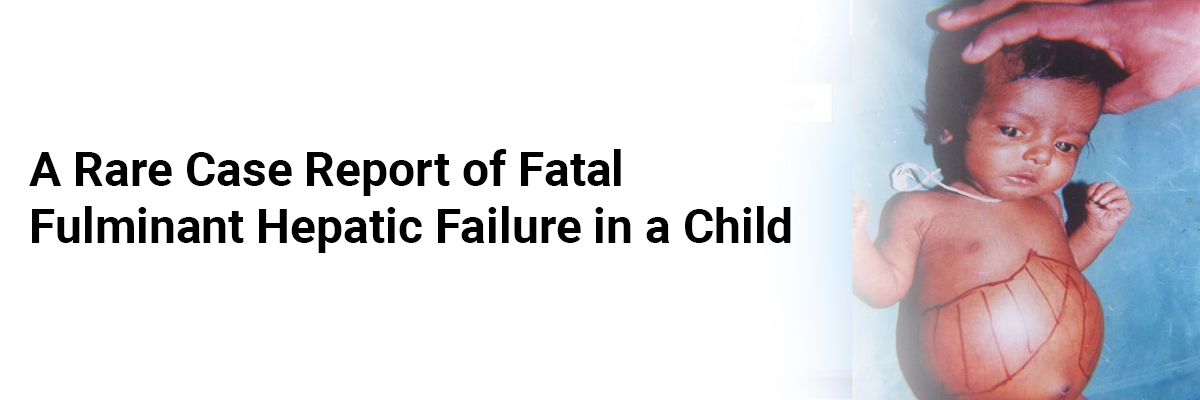
A six-year-old female child, presented with fever for four days, yellowish discoloration of eyes, and urine for two days, progressive swelling of whole body starting from feet for one day. Fever was moderate to high grade, intermittent in type associated with chills and rigor subsided with medication and profuse sweating. There was no history of black coloured stools, vomiting, bleeding from any site, and any change in conscious level, jaundice in the past, any history of blood transfusion, and intravenous medication in the past or any history of drug intake. There was no history suggestive of respiratory tract infections, skin infection, decreased micturition, and reddish coloured urine. There was no significant past, antenatal, perinatal, or family history. The child was fully immunized, conscious, cooperative, and orientated and was on regular diet. At admission her pulse was 78 per minute, respiratory rate 26 per minute, and blood pressure 98/68 mm of mercury. There were severe pallor, and icterus. Lymph nodes were not palpable. Abdominal examination reveals that liver was palpable 4 cms below costal margin with span of 10 cm the spleen was palpable 1 cms below costal margin. Her respiratory, cardiovascular (CVS), and central nervous system (CNS) examination was normal. Haematological investigations reveals haemoglobin (4.9 g/dL), total leucocyte count (10.6 × 103 per µL with polymorphs 54%), lymphocytes (42%), monocyte (4%), platelet count (11×103 per µL) and erythrocyte sedimentation rate (8 mm/1st hour by Westergren method). Blood sugar was 84 mg/dL. Total serum bilirubin was 27.5 mg/dL, indirect fraction of 18 mg/dL. SGOT was 495 and SGPT 210. Serum total protein was 2.8 gram (gm) and albumin 1 gm per 100 mL of blood. Blood urea nitrogen was 189 mg/dL, creatinine 0.6 mg/dL, sodium 136 meq/L, potassium 4.1 meq/L. Prothrombin time was 17.3/12 with INR of 1.44. Viral markers (HBsAg, IgM hepatitis C, A and E) were negative. Chest X-ray was normal and ultrasonography abdomen showed hepatosplenomegaly. On peripheral smear trophozoites and schizonts of P. vivax and trophozoites and gametocytes of P. falciparum were seen. Rapid malarial antigen test was positive. Arterial blood gas analysis showed pH 7.45, partial pressure (PP) of oxygen 104, PP of carbon dioxide 45, and standard bicarbonate 28 meq/L. Urine routine and microscopy were normal.
She was given injection of Artesunate 2.4 gm/kg body weight, along with cefotaxime and vitamin K. She received fresh frozen plasma, packed red cell, platelets along with inotropes. Within five hours of admission she developed profuse upper gastrointestinal bleeding, along with deterioration of consciousness. She went into shock, then cardiorespiratory arrest from which she could not be revived.
Discussion
Jaundice is one of the common severe manifestations of falciparum malaria. Severe malaria due to P. falciparum may pretense as FHF. Simple clinical and laboratory parameters can easily distinguish severe malaria from FHF.
Causes of Jaundice in Malaria are divided into three categories i. e. direct causes (malarial hepatitis, intravascular hemolysis of parasitized RBC, and septicemic hepatitis), indirect causes: microangiopathic hemolysis associated with DIC, G6PD-related hemolysis, and anti-malarial-drug induction), unrelated causes (coexisting acute viral hepatitis).
Early diagnosis of malarial can be treated with quinine, whereas liver transplantation may be required for FHF in selected patients. The management of malarial hepatitis is similar as the management of severe malarial infection. In endemic areas, it is expected to have infection with malarial parasite presenting as FHF. Since the clinical presentation is misleading, laboratory help may be needed to establish the etiology of malarial hepatitis. Repeated smears are more reliable to pick up the diagnosis. Treatment of severe malaria is artesunate or quinine intravenously till the child becomes conscious followed by oral treatment for a total of seven days.
Suggested Reading
- Mehta SR, Naidu G, Chandar V, Singh IP, Johri S, Ahuja RC. Falciparum malaria--present day problems. An experience with 425 cases. J Assoc Physicians India. 1989;37(4):264-267.
- Cook GC, “Malaria: an underdiagnosed and often neglected medical emergency,” The Australian and New Zealand Journal of Medicine, vol. 22, no. 1, pp. 69–82, 1992.
- Echeverri M, Tobón A, Alvarez G, Carmona J, Blair S. Clinical and laboratory findings of Plasmodium vivax malaria in Colombia, 2001. Rev Inst Med Trop Sao Paulo. 2003;45(1):29-34.
- Rupani AB, Amarapurkar AD. Hepatic changes in fatal malaria: an emerging problem. Ann Trop Med Parasitol. 2009;103(2):119-127.

IJCP Editorial Team
Comprising seasoned professionals and experts from the medical field, the IJCP editorial team is dedicated to delivering timely and accurate content and thriving to provide attention-grabbing information for the readers. What sets them apart are their diverse expertise, spanning academia, research, and clinical practice, and their dedication to upholding the highest standards of quality and integrity. With a wealth of experience and a commitment to excellence, the IJCP editorial team strives to provide valuable perspectives, the latest trends, and in-depth analyses across various medical domains, all in a way that keeps you interested and engaged.




















Please login to comment on this article