 IJCP Editorial Team
IJCP Editorial Team
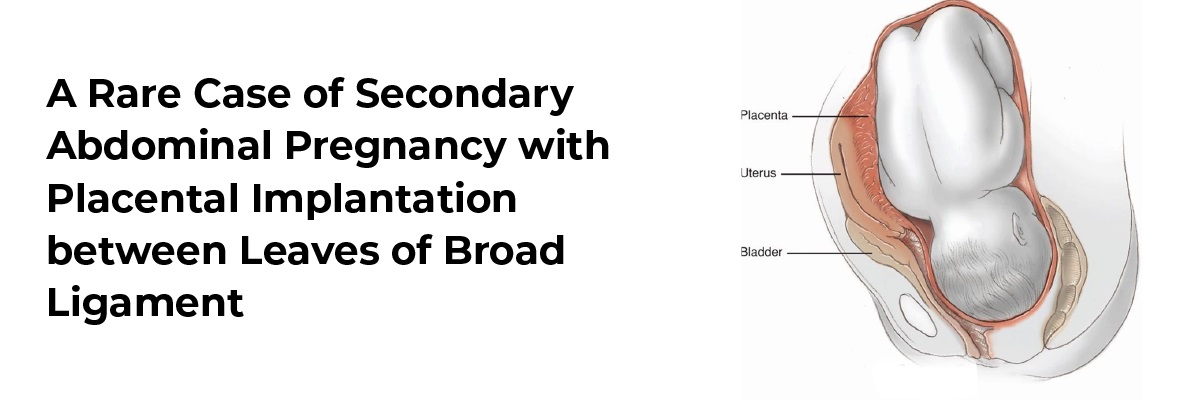
A Rare Case of Secondary Abdominal Pregnancy with Placental Implantation between Leaves of Broad Ligament
Abdominal pregnancy has historically been defined as implantation in the peritoneal cavity, exclusive of tubal, ovarian, or intraligamentary pregnancy. Abdominal pregnancy is a rare obstetric complication with high maternal mortality and even higher perinatal mortality, and it can be primary or secondary with the latter being the most common type. Primary peritoneal implantation is rare.
Secondary abdominal pregnancy almost always follows the early rupture of a tubal ectopic pregnancy into the peritoneal cavity with the incidence being 1 in 10,000 live births. Advanced abdominal pregnancy is rare and accounts for 1 in 25,000 pregnancies. Risk factors for abdominal pregnancy are the same as for ectopic pregnancy and, when it is recognized, immediate laparotomy with removal of the fetus is usually recommended. The present identifies a case of secondary abdominal pregnancy with placental implantation between leaves of the broad ligament.
The case subject, a 32-year-old, with the third gravida presented with 8 months of pregnancy with 2 live issues reported intrauterine death, ascites, and poor general condition. During the antenatal period, the patient complained of pain abdomen at 2 months of gestational age. The USG report showed 8 weeks live gestation, fetal cardiac activity, and fetal movements. Mild free fluid was also present in the pelvis along with inflamed bowel loops. Further, the patient continued to have dull aching pain abdomen throughout her pregnancy, with acute exacerbations off and on. Another USG report after 2 months showed a single live fetus of 23 weeks with regular cardiac activity and placenta in the right lateral position, grade1.
The patient was brought to the hospital after experiencing the third episode of exacerbation with a history of severe pain abdomen, two episodes of vomiting, and abdominal distention for 1 day. Her USG report showed a single dead fetus of 31 weeks and maternal ascites with a few septations. On examination, the patient was dyspneic and unable to lie down due to pain abdomen. On per abdominal examination, the uterus was 34 weeks in size. Tenderness was present in the epigastrium and right lumbar area. Also. fetal parts could not be assessed and fetal heart sounds could not be heard. On opening the abdomen, about 3.5 liters of hemoperitoneum was found. Placenta was found implanted between the leaves of the broad ligament and bleeding was present from the placental site. Hence, a hysterectomy was performed.
The doctors concluded that the patient probably had a cornual pregnancy which ruptured around 8 weeks, followed by which the placenta got implanted between the two leaves of the broad ligament, while the fetus continued to grow intra-abdominally in an intact amniotic sac.
Ultrasound, magnetic resonance imaging (MRI), computed tomography (CT) scan, and laparotomy can help in differentiating between primary and secondary abdominal pregnancy. Proper pre-operative evaluation with appropriate diagnostic techniques can help with a timely diagnosis. Pre-operative treatment such as methotrexate is recommended at all gestational ages to minimize blood loss at surgery and can facilitate maximal placental removal.
Source
- Cunningham FG, Gant NF, Leveno KJ et al (eds). Williams Obstretrics21st edn New York, McGraw Hill. 2001:899.
- Shaw HA, Ezenwa E : Secondary abdominal pregnancy in a Jehovah’sWitness. Southern Medical Journal 2000; 93:898-900.
- Rahman MS, Suleiman A, Al-Sibai MH et al. Advanced Abdominal Pregnancy – Observations in 10 Cases. Obstet Gynecol 1982;59:366-72.
- Martin JN, Sessums K, Martin RW et al. Abdominal pregnancy –currentconcepts of management Obstet Gynecol 1988;71:549-57.
- Worley KC, Hnat MD, Cunningham FG: Advanced extra uterine pregnancy: diagnostic and therapeutic challenges. Am J Obstet Gynecol 2008, 198:297.e1-297.e7. PubMed Abstract |Publisher Full Text
- Studdiford WE: Primary peritoneal pregnancy. Am J Obstet Gynecol 1942, 44:487-491.
- Atrash HK, Friede A, Hogue CJ: Abdominal pregnancy in the United States. Frequency and maternal mortality. Obstet Gynecol 1987, 69:333. PubMed Abstract

IJCP Editorial Team
Comprising seasoned professionals and experts from the medical field, the IJCP editorial team is dedicated to delivering timely and accurate content and thriving to provide attention-grabbing information for the readers. What sets them apart are their diverse expertise, spanning academia, research, and clinical practice, and their dedication to upholding the highest standards of quality and integrity. With a wealth of experience and a commitment to excellence, the IJCP editorial team strives to provide valuable perspectives, the latest trends, and in-depth analyses across various medical domains, all in a way that keeps you interested and engaged.






















Please login to comment on this article