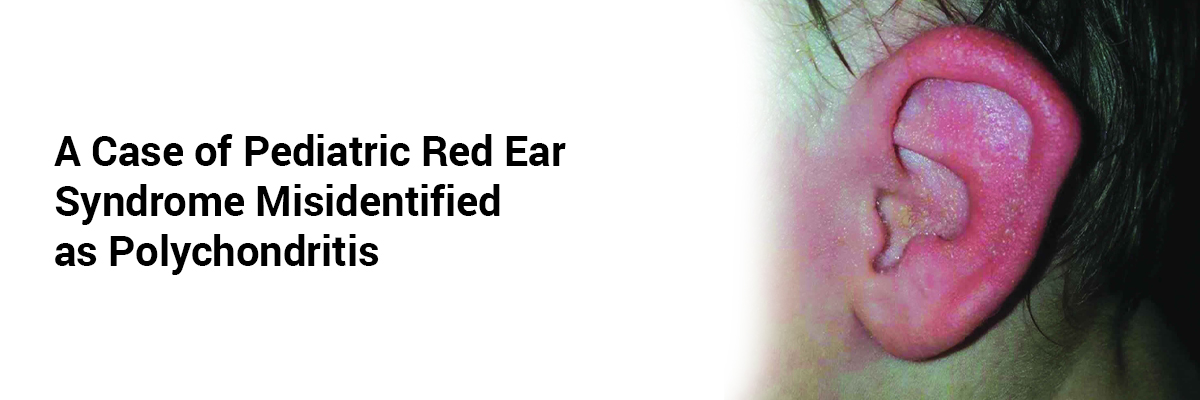
A Case of Pediatric Red Ear Syndrome Misidentified as Polychondritis
Red
ear syndrome (RES) is a rare condition characterized by recurrent episodes of
ear redness and burning pain. It is more commonly reported in adults, with
pediatric cases being uncommon and often misdiagnosed.
A
14-year-old boy presented with a five-year history of recurrent severe left ear
pain and erythema, initially misdiagnosed and treated as relapsing
polychondritis (RP). The patient's symptoms began five years
ago with sudden burning pain over the ear, radiating to the cheek. Episodes
ranged from 10 minutes to six hours and sometimes involved constant aching.
Attacks occurred in clusters lasting up to four months.
Despite
various immunosuppressive treatments—including corticosteroids, pregabalin,
dapsone (discontinued due to allergy), Imuran, colchicine, tocilizumab, and
adalimumab—his symptoms persisted and worsened, leading to frequent school
absences.
Upon
reevaluation, physical examination revealed isolated unilateral auricular
erythema and burning sensation, with no neurological deficits. Investigations
showed elevated CRP and ESR but a negative autoimmune workup and normal MRI.
Based on clinical features and the exclusion of other causes, a diagnosis of
idiopathic respiratory eosinophilia syndrome (RES) was made.
The
patient was started on ibuprofen, a tricyclic antidepressant, and a calcium
channel blocker. Over the following months, he experienced a marked reduction
in attack frequency and intensity, with complete resolution by the 3-month
follow-up and sustained remission through the one-year mark.
This
case highlights the importance of recognizing respiratory distress syndrome
(RDS) in children to avoid misdiagnosis and inappropriate treatment. There is a
need for greater awareness and research into effective therapies.
(Source:Case reports in pediatrics vol. 2025 6464822. 20 Jan. 2025,
doi:10.1155/crpe/6464822;https://onlinelibrary.wiley.com/doi/full/10.1155/crpe/6464822)














Please login to comment on this article