Abstract
Meningococcal pericarditis is a rare and potentially life-threatening
complication of Neisseria meningitidis infection, typically occurring
in the setting of disseminated meningococcal disease. We present a case of
meningococcal pericarditis in an adult with purpura fulminans, highlighting the
diagnostic challenges and need for prompt management.
Introduction
Meningococcal pericarditis is classified into three clinical types:
1. Purulent
pericarditis – due to direct bacterial invasion
2. Immunologic
pericarditis – due to immune-mediated inflammation
3. Chronic
constrictive pericarditis – a late sequela
Although Neisseria meningitidis commonly presents with meningitis
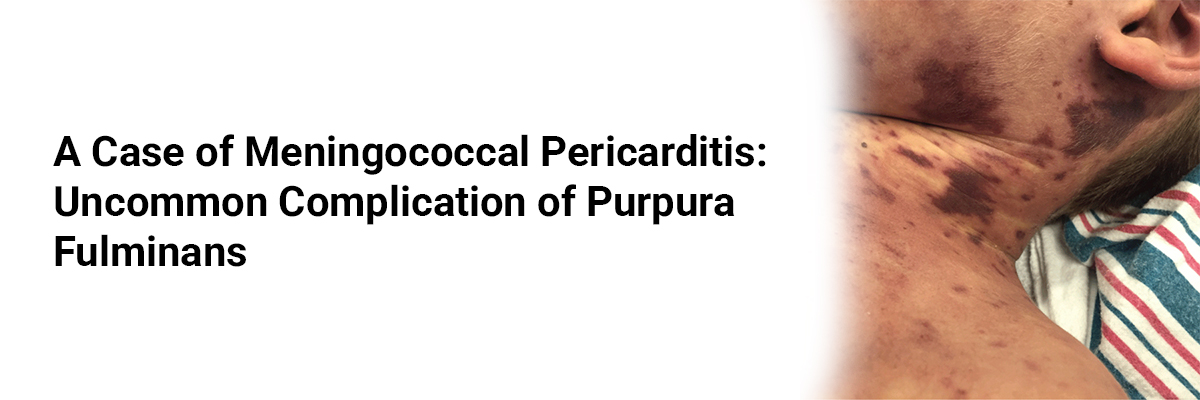
or septicemia, cardiac involvement is rare. Purpura fulminans, characterized by
rapidly progressive cutaneous hemorrhagic necrosis, indicates severe sepsis and
carries a high mortality risk.
Case Presentation
A 32-year-old previously healthy male presented with high-grade fever,
malaise, and rapidly progressive purpuric rash over the extremities.
He developed hypotension and altered mental status within hours of admission.
On examination:
·
BP: 80/50 mmHg, HR: 120 bpm
·
Extensive purpura over lower limbs and trunk
·
Muffled heart sounds and distended neck veins
·
Signs of septic shock
Investigations:
·
CBC: Leukocytosis with neutrophilia
·
Coagulation profile: Prolonged PT and aPTT, low
fibrinogen
·
Blood cultures: Neisseria meningitidis
serogroup C
·
Echocardiography: Large pericardial effusion
with early tamponade features
·
Skin biopsy: Dermal vessel thrombosis with
fibrin deposition (consistent with purpura fulminans)
Management:
The patient received aggressive fluid resuscitation, broad-spectrum intravenous
antibiotics (ceftriaxone), vasopressor support, and fresh frozen plasma for
disseminated intravascular coagulation. Pericardiocentesis drained 500 mL of
purulent fluid, which also grew N. meningitidis.
Outcome:
Despite initial stabilization, the patient required prolonged ICU stay due to
multi-organ dysfunction. Over the following weeks, skin necrosis over both
lower limbs necessitated surgical debridement. He was discharged after 28 days
with preserved cardiac function and no evidence of constrictive physiology on
follow-up echocardiography.
Discussion
Meningococcal pericarditis is rare but should be considered in patients with
meningococcal septicemia who develop new cardiac symptoms or hemodynamic instability.
Purpura fulminans reflects severe endotoxin-mediated vascular injury and
carries a poor prognosis without rapid intervention.
Early echocardiography and timely pericardial drainage are critical to prevent
tamponade-related mortality. In this case, concomitant pericardial infection
and severe coagulopathy posed significant management challenges.
Conclusion
Meningococcal pericarditis, though uncommon, can complicate the course of
purpura fulminans and septicemia. Clinicians should maintain a high index of
suspicion for cardiac involvement in severe meningococcal disease, enabling
timely diagnosis and life-saving intervention.














Please login to comment on this article